I had a great experience, the staff are super nice and very informative. They made sure i was fine and asked if i had any questions, the surgery itself went perfectly smooth. I would recommend them to anyone needing oral surgery. Definitely had a positive experience.
General Information
What is Orthognathic Surgery?
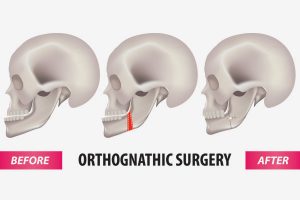 Orthognathic surgery (Corrective Jaw Surgery) is needed when jaws don’t meet correctly and/or teeth don’t seem to fit properly. Teeth are straightened with orthodontics and corrective jaw surgery repositions the misaligned jaws. This not only improves facial appearance, but also ensures that teeth meet correctly and function properly. If your dentist or orthodontist feels you are a candidate for orthographic surgery, an oral maxillofacial surgeon is needed in your treatment plan.
Orthognathic surgery (Corrective Jaw Surgery) is needed when jaws don’t meet correctly and/or teeth don’t seem to fit properly. Teeth are straightened with orthodontics and corrective jaw surgery repositions the misaligned jaws. This not only improves facial appearance, but also ensures that teeth meet correctly and function properly. If your dentist or orthodontist feels you are a candidate for orthographic surgery, an oral maxillofacial surgeon is needed in your treatment plan.
Who Needs Orthognathic Surgery?
People who can benefit from orthognathic surgery include those with an improper bite or whose jaws are positioned incorrectly. Jaw growth is a gradual process, and in some instances, the upper and lower jaws may grow at different rates. When one or both jaws do not grow at the same rate and the teeth do not fit together the result can be a host of problems that can affect chewing function, speech, long-term oral health, and appearance. Injuries to the jaws or birth defects can also affect jaw alignment. While, orthodontics alone can correct many bite problems when, orthognathic surgery may be required if there is a skeletal discrepancy.
Difficulties In The Following Areas Should Be Evaluated:
- Difficulty in chewing, biting or swallowing
- Speech problems
- Chronic jaw or TMJ pain
- Open bites
- Protruding jaw
- Breathing problems
Before any treatment begins, a consultation will be held to perform a complete and thorough examination
How Is The Surgery Performed?
Accurate radiographs, three dimensional models and modern computer imaging will be used by your doctor to determine if you are a candidate for orthognathic surgery and how your surgery will be performed. This technology will also show you how your bite will be improved and even give you an idea of how you will look after surgery. This helps you understand the surgical process, the extent of the treatment prescribed, and to see the benefits of orthognathic surgery. Upper or lower jaw surgery (or sometimes both) may be necessary to achieve the jaw function and facial balance.
If you are a candidate for corrective jaw surgery, your surgeon will work closely with your orthodontist during your treatment. Your orthodontist will straighten your teeth with braces first. Jaw surgery will be performed afterwards by your surgeon who will move the jaws into the optimum position. The actual surgery can move your teeth and jaws into a new position that results in a more attractive, functional and healthy dental-facial relationship.
Jaw surgery is routinely performed in the hospital under a general anesthetic. The surgeries are performed from the inside of the mouth and rigid fixation (plates and screws) are used to hold the jaws in the correct position. Most patients stay in the hospital for one or two days after the surgery. See the Orthognathic Surgery: Pre-operative & Post-operative Instructions.
Your doctor will thoroughly explain your individual instructions before and after surgery. Your doctor will see you multiple times before and after your surgery.
